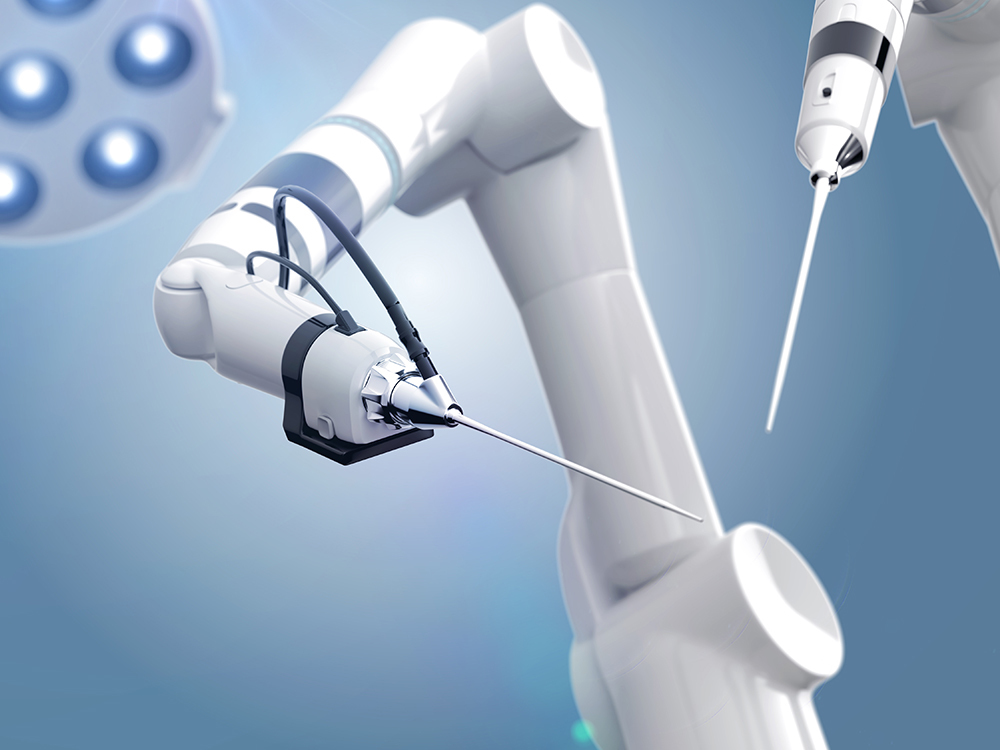
Interventions in spinal surgery require absolute sure instincts from the surgeon. A miniature hexapod with 6 degrees of freedom, which is used as a guidance aid, offers high-precision assistance. The SpineAssist system is fixed to the bone and allows absolute precision when inserting implants to stabilize spinal fusions in open and minimally invasive surgical procedures.
The system includes a preoperative planning software package that supports automated fluoroscopic and CT image processing, and a set of rigid bone fixation clamps and platforms.
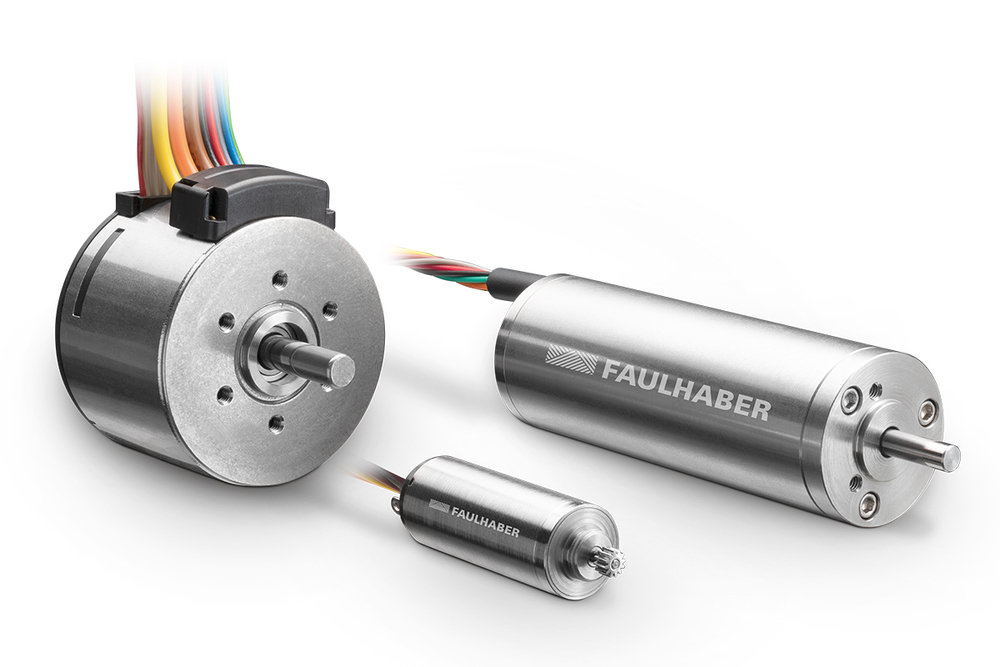
Mazor Surgical Technologies, inventor of the SpineAssist system and founder of the surgical method it is based on, was established in 2001 as a spin-off from the Mechanics Department of the Institute of Technology, Israel. The company has offices in Caesarea, Israel and in Norcross, Georgia, USA (Mazor Surgical Technologies Inc.). Mazor has specialized in the development of medical robotic systems, whereby the manufacture of the precision mechanical parts has been outsourced to the Swiss company MPS Micro Precision Systems AG, a member of the FAULHABER Group.
Accuracy is of the utmost importance when placing implants in spinal surgery, as procedures are primarily performed in the vicinity of nerve roots and the spinal cord and every millimeter can be crucial. For this reason, and also due to other biomechanical requirements, precision and accuracy are of the utmost importance in this type of intervention.
Spinal fusion is a surgical intervention used, for example, to straighten the spine to counteract progressive deformity due to scoliosis or similar conditions.
The procedure is also used to support a weak or damaged spine or to counteract or relieve pain from pinched or worn nerves. Although spinal fusions achieve remarkably high success rates, the incidence of implant misplacement is alarmingly high. According to some sources, these occur in up to 25% of scoliosis-related procedures. Misplacement is associated with an increased risk of neural and vascular complications and spinal cord injury.
The intervention using SpineAssist consists of five steps: 1) preoperative planning phase, based on a CT scan of the spine; 2) rigid fixation of the SpineAssist platform to the patient's spine; 3) position calibration by matching a fluoroscopic image of the bone assembled platform with a CT scan from the preoperative planning phase;4) Rigid fixation of the SpineAssist robot to the platform;5) Accurate automatic positioning of the robotic guide arm using the information from the preoperative plan to guide the surgeon during drilling and others interventions. The SpineAssist procedure is FDA cleared, CE marked and has been clinically tested in 250 cases worldwide to date.
Minimally invasive surgery (MIS) is one of the most significant developments in the medical device industry today. The potential advantages of minimally invasive procedures are manifold: A smaller incision - and therefore smaller scarring - reduces the risk of infection and bleeding. In addition, the use of minimally invasive procedures can reduce postoperative pain and trauma and shorten hospital stays and recovery times; one of the reasons why the medical device industry is constantly working on the development of new instruments that are used in the field of minimally invasive surgery.
The SpineAssist system enables spinal fusion procedures to be performed with only a few small incisions, while the comparably large incisions that traditional surgical methods require can result in potential muscle damage. The particularly small dimensions of the robot, the fact that no direct view is required and the high precision of the method facilitate the surgical procedure and minimize the risk of misplaced screws. Since the robot is rigidly fixed to the patient, no coordinate tracking system is required. With SpineAssist, the procedure requires only a small number of fluoroscopic exposures, adding another significant benefit to reduced radiation exposure for the surgeon and patient.
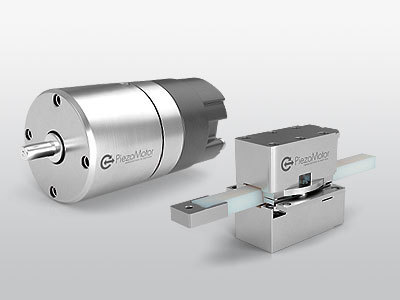
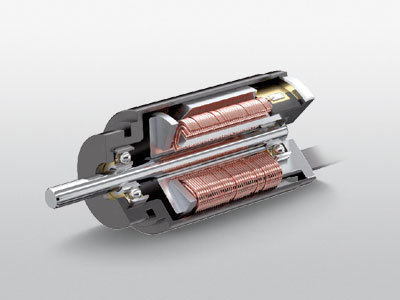
The SpineAssist robot
The mini